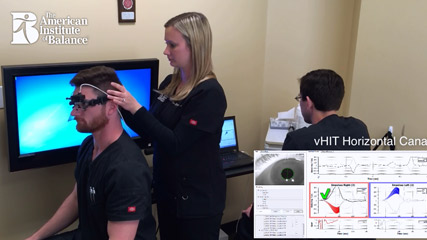
VIDEO- Video Head Impulse Test (vHIT) Has High Diagnostic Sensitivity and Provides VRT Outcome Validation
Published on: December 18, 2014
Clinicians and therapists have historically been limited by the constraints of caloric testing, which is a very poor indicator of comprehensive VOR function due to its testing of only the horizontal canals at ultra low-frequency sensitivity (.003Hz). More importantly, caloric testing cannot provide the status of the patient’s compensation. For patients with mid-high frequency non-compensated unilateral vestibulopathy (UVD) secondary to disease or trauma, this has caused many to go undiagnosed, untreated or unable to demonstrate VRT efficacy without an objective measurement. The vHIT is a relatively new measurement to record head and eye velocity. Conducting the vHIT allows clinicians the ability to evaluate all six semicircular canals using the natural physiologic stimuli of the head impulse. This technology is far more sensitive than the classic bedside Head Impulse Test that has long been recognized as an excellent clinical assessment tool.
Clinical application includes:
- Evaluation of UVD post disease-disorder or trauma.
- Expands the range of VOR testing for all six canals and into a normal head movement frequency range with greater sensitivity.
- Use when caloric or rotary chair testing is unavailable or contraindicated.
- Demonstrate central compensation pre-post VRT to better triage therapy and to determine return to play (RTP) or work activities.
- Pediatric population when caloric or rotary chair is not available or contraindicated.
AIB is incorporating vHIT into its protocols in conjunction with c-VEMP, rotary Chair, Active Head Rotation, and Dynamic Visual Acuity (DVA) tests, in order to ensure that patients with chronic dizziness, Oscillopsia and imbalance receive the most comprehensive examination, always with the purpose of developing and implementing the most effective and efficient VRT treatment protocols using Diagnosis Based Strategies, specific to the patient’s functional impairment.
References:
1. Dispenza, F. and DeStefano, A., (Ed.) 2014, Textbook of Vertigo Diagnosis and Management, Jaypee Brothers Medical Publishers, London
2. http://www.ncbi.nlm.nih.gov/pubmed/23630593
4. http://www.neurology.org/content/70/6/454.short